The AAN Brain Health Summit 2025 Proceedings Summary
AAN Brain Health Initiative
Overview
The AAN hosted the fourth annual Brain Health Summit in fall 2025. The summit brought together 175 thought leaders representing over 90 organizations from across academia, research, government, industry, advocacy, and beyond to collectively tackle the most significant challenges and pursue key opportunities in the field of brain health.
Themed “Empowering Communities,” the summit showcased speakers with real-life experience as caregivers and advocates for those with neurological diseases, as well as scientific experts and practitioners in the areas of cutting-edge gene therapy, community-engaged participatory research, implementation and translational science, health equity, public policy, and mental health. Summit attendees participated in two small breakout group discussions and heard from leaders across the house of medicine representing the AAN, the Council of Medical Specialty Societies, the American Academy of Family Physicians, the American Academy of Pediatrics, and the American Psychiatric Association.
The 2025 Brain Health Summit was led by AAN President Natalia S. Rost, MD, MPH, FAAN, FAHA; Brain Health Committee Chair David A. Evans, MBA, DAAN; and Brain Health Committee Vice Chair Rana R. Said, MD, FAAN.
This summary documents the summit’s annual program for future reference.
View the 2025 Brain Health Summit program booklet and attendee list.
The next AAN Brain Health Summit will take place on September 17, 2026, in Washington, DC. Please contact brainhealth@aan.com with any questions.
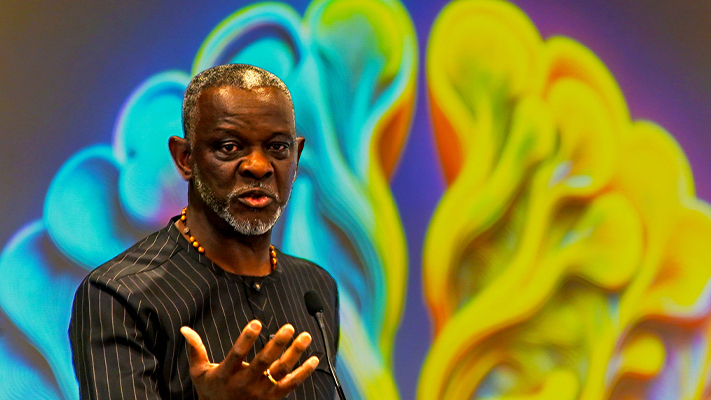
Speaker Gbenga Ogedegbe, MD, MPH, FACP, delivers his keynote presentation.

Summit attendees participate in small breakout group discussions.

Summit keynote presentation speakers participate in an open forum. From left, Gbenga Ogedegbe, MD, MPH, FACP, Katie Brandt, MM, and Laura Erickson-Schroth, MD, MA.

Speaker Joel Salinas, MD, MBA, MSc, FAAN, delivers his keynote presentation.

Summit attendee Mohita Kumar, MD, participates in small breakout group discussion.

Summit attendee Diana Slowiejko, PharmD, PhD, participates in small breakout group discussion.

Rana R. Said, MD, FAAN, AAN Brain Health Committee Vice Chair, facilitates the small group discussions.
Keynote speaker presentation summaries
 From Caregiver to Catalyst: Empowering Communities Through Story and Science
From Caregiver to Catalyst: Empowering Communities Through Story and Science
Katie Brandt of shared her transformative journey from caregiver to advocate, highlighting the power of personal experience in driving caregiver and community empowerment for brain health. Drawing on her experience as a caregiver for loved ones impacted by dementia, Brandt emphasized the importance of recognizing early signs and symptoms, building connections among patient families, and fostering partnerships with advocacy organizations. She underscored the value of digital communication channels and engagement boards to strengthen support networks. Brandt advocated for the use of storytelling and scientific knowledge to inspire action and discussed how volunteer roles and recognition can empower caregivers. Her presentation concluded with gratitude for the individuals and organizations supporting her mission, and an invitation to explore her podcast, which addresses care for those affected by frontotemporal disorders, Alzheimer’s disease, and related dementias.
 Changing DNA to Change Lives: Innovation for Brain Health
Changing DNA to Change Lives: Innovation for Brain Health
Patricia Musolino, MD, PhD, from Massachusetts General Hospital and Harvard Medical School, presented in genetic medicines for brain and vascular health. Her presentation highlighted the development and application of gene therapy and genome editing for rare and common cerebrovascular diseases. She covered the genetic research cycle, therapeutic modalities, and the translation of these innovations from preclinical models to clinical trials. Her presentation emphasized the need for targeted, long-lasting, and safe therapies, the challenges of current standard-of-care treatments, and the promise of novel delivery vectors for efficient gene editing in vascular cells. The ultimate goal is to restore vessel health, improve patient outcomes, and enable personalized, accessible genomic therapies for brain health disorders. Musolino concluded by asking the audience to imagine changing DNA in a safe, accessible, and sustainable manner to equalize access to brain health; for every child, one child at a time.
 Advancing Brain Health: Translating Research into Practice with Minoritized Populations
Advancing Brain Health: Translating Research into Practice with Minoritized Populations
Gbenga Ogedegbe, MD, MPH, FACP, from NYU Grossman School of Medicine, presented a keynote presentation focused on reducing stroke disparities among Black and Hispanic stroke survivors. Ogedegbe highlighted the disproportionate burden of stroke among Black and Hispanic populations and the central role of social determinants of health in addressing disparities. Drawing on pragmatic trials, he reported that produced significantly greater reductions at 12 months, though this did not lower recurrent stroke at 24 months, pointing to the need for longer-term, community-embedded strategies. yielded meaningful declines of nearly 10 mmHg, showing the power of routine support, while enhanced transitional care and health coaching revealed that adding clinical layers may be insufficient without deeper community integration. A third trial found that improved preparedness among participants with low education, underscoring the value of context-specific interventions for this population. Ogedegbe concluded that scaling health equity-focused strategies rooted in community realities is essential to meaningfully address stroke disparities.
 DPRIT: When Public Policy Chases a Cure
DPRIT: When Public Policy Chases a Cure
Matt Dowling of the presented on the creation and passage of the Dementia Prevention Research Institute of Texas (DPRIT), a landmark 10-year, $3 billion state initiative to accelerate research and prevention efforts for dementia, Alzheimer’s disease, Parkinson’s disease, and related disorders. He described the legislative hurdles and political dynamics in Texas, where public health funding is often limited, and emphasized how persistent advocacy and compelling testimony from patients, families, and physicians shaped DPRIT’s success. He drew parallels to the Cancer Prevention Research Institute of Texas (CPRIT), which produced Nobel Prize-winning research, expanded cancer services, and attracted top scientists to the state. DPRIT is expected to bring similar breakthroughs and economic impact while addressing urgent brain health needs for patients and caregivers. Dowling underscored positioning Texas as a national leader in brain health at a time when federal funding is uncertain.

Supporting the Mental Health of the Digital Generation
Psychiatrist Laura Erickson-Schroth, MD, MA, of , spoke about brain health encompassing both cognition and mental health, highlighting their interconnectedness and the shared factors that affect both, such as exercise and social connection. She argued that the digital world and the rise of AI are profoundly impacting young people, changing how they engage with news and form community. She cautioned against the unmonitored use of AI companions, citing risks to mental health, and called for intentional legislative action to regulate AI with hard-coded safety protocols. Ultimately, she asserted that the key to protecting the brain health of the next generation lies in preserving two fundamental human traits: critical thinking and social connection, urging her audience to actively foster these skills in the young people in their lives.
 Empowering Families, Driving Progress
Empowering Families, Driving Progress
Amanda Moore, MA, is CEO of the and mom to 9-year-old Jackson, who has Angelman syndrome (AS). She presented on AS and highlighted the disorder’s genetic cause, symptoms, and current treatment landscape. She emphasized the importance of building a supportive community and driving change based on family inclusion and partnership. The Linking Angelman and Dup15q Data for Expanded Research (LADDER) Learning Network connects patients to care, supports clinical trials, and leverages patient data for therapy development. Moore discussed challenges such as the need for sustained investment in clinics and infrastructure, and the gap between urgent family needs and the slower pace of scientific progress. Her call to action included three recommendations: Support Extension for Community Healthcare Outcomes (ECHO) Project programs to expand access to expert AS care, be ready to engage with new initiatives, and partner closely with families to ensure their perspectives shape care and support.
Leadership Speaker Panel
From Collaboration to Action: Leading Across the House of Medicine
- Helen Burstin, MD, MPH, MACP – CEO,
- Mark Del Monte, JD – CEO and Executive Vice President,
- R. Shawn Martin – Executive Vice President and CEO,
- Theresa Miskimen Rivera, MD – President,
- Mary E. Post, MBA, CAE – CEO, 好色先生
- Moderated by David A. Evans, MBA, DAAN – CEO,

Five leaders from major medical organizations discussed how collaboration across specialties can advance brain health. Panelists shared examples of successful partnerships, highlighted the need to break down silos, and emphasized the importance of integrating brain health into all areas of care. They addressed opportunities in neurology, psychiatry, family medicine, pediatrics, and other specialties, stressing that collective action and shared leadership are essential to advance brain health for all at every stage of life.
Breakout sessions
Session one: Community engagement
Before attendees participated in the summit’s first breakout session, , the chief medical officer at Isaac Health, presented on the importance of prioritizing community engagement as the foundation for effective strategies to promote brain health.
Attendees, seated at tables assigned by chosen life stage of interest (fetal/childhood development, youth/adolescence, adulthood, maturity, and senescence), were asked to complete this sentence as a group: “Our brain health public health message is X, through Y, for population Z.” Examples include:
Fetal/childhood development
- Set your baby's brain up for success through quality time and quality foods. This message is intended to speak universally to parents and to encourage a focus on fetal health by slowing down, eating together, and building healthy habits for their child’s growing brain.
Youth/adolescence
- Concussion is brain injury; when do I return to play? Delivered by training booster club members at home games to educate rural K–12 athletes and provide screening tools for referral.
Adulthood
- It’s never too late to help your brain; small changes can grow big. Delivered through community organizations, food banks, libraries, job fairs, and pharmacies to reach populations of people who might be living with one or more high risk conditions.
Maturity
- Mind your brain. Delivered through community faith institutions and faith leaders for culturally specific senior communities, including family and caregivers, to raise awareness and promote cognitive screening.
Senescence
- Aging well means connecting with community, movement, sleeping well, building purpose, and regular brain health checks. Delivered through primary care, neurology, pharmacies, community centers, senior centers, faith partners, and bilingual media for adults 65+ and their caregivers, especially in under-resourced communities.
All life stages
- It’s never too late—or too early—to improve your brain health. Delivered via targeted media, resource development and distribution by the AAN, and community ambassadors; targeting families, community leaders, legislators, neurologists, and primary care providers.
- Caregivers for those living with brain-related conditions are superheroes. Delivered through advocacy, public education, community engagement, and policy reform.
 Session two: Clinical trials and community implementation opportunities
Session two: Clinical trials and community implementation opportunities
Before attendees participated in the summit’s second breakout session, , senior vice president of medical and scientific relations at the Alzheimer’s Association, presented on the recently published study results of the .
Attendees were asked to answer this question as a group: “What are one to two implementation opportunities that might exist to translate a rigid clinical trial to a pragmatic community setting?” Examples include:
Fetal/childhood development
- Start early: Begin interventions early, even prenatally when feasible, and emphasize clear, evidence-based outcomes to illustrate their impact.
- Break up interventions: Divide elements into smaller, manageable pieces.
- Leverage community health workers and local spaces: Pharmacies, etc.
- Gamification and community engagement: Use games and involve parents/peers to improve motivation and provide social support.
Youth/adolescence
- 好色先生al videos: Use popular characters (Marvel, KPop Demon Hunters) or athletes to teach about health topics (e.g., concussion symptoms) in schools, clinics, and sports settings.
- Cross-group partnerships: Collaborate with other chronic condition groups for shared education and wellness goals.
- Family and care system engagement: Educate the entire family and care system for community buy-in.
- Leverage organized social groups: Schools, sports teams, faith-based organizations as champions and communication conduits.
Adulthood
- Empower local resources: Equip primary care practitioners and community health workers, alumni, and trusted community resources (e.g., barbershops).
- Economic measures: Develop local economic metrics to advocate for funding and policy changes.
- Community leader engagement: Improve acceptance and compliance.
- Cultural adaptation: Address priorities and access issues by aligning with local leadership and values.
Maturity
- Annual cognitive screening: Offer and incentivize screenings through primary care practitioners and in nonmedical settings.
- Patient incentives: Motivate continued participation after study completion.
- Trusted influencer amplification: Use trusted influencers for accurate messaging and behavior change.
- 好色先生 and empowerment: Educate patients about trials and empower them to ask questions.
Senescence
- Small clinics in rural settings: Start interventions in accessible locations.
- Community organization partnerships: Build on existing organizations, family resource centers, faith institutions, and community health workers.
- Barriers: Remove barriers to connecting with medical teams (remote/home visits) and foster mutual respect between clinical and community groups.
- Memory care hubs: Create community-based hubs for memory care.
All life stages
- Community access points: Use health centers, groceries, pharmacies, gas stations, and schools for program delivery.
- Digestible information: Provide information in bullet points and graphics.
- Opt-in biometric data sharing: Enhance community exercise programs with data sharing.
- Community engagement: Build relationships early with stakeholders and educate on trial results.
These responses are those identified by individual summit attendees and do not necessarily represent the views of all meeting participants or the AAN.
